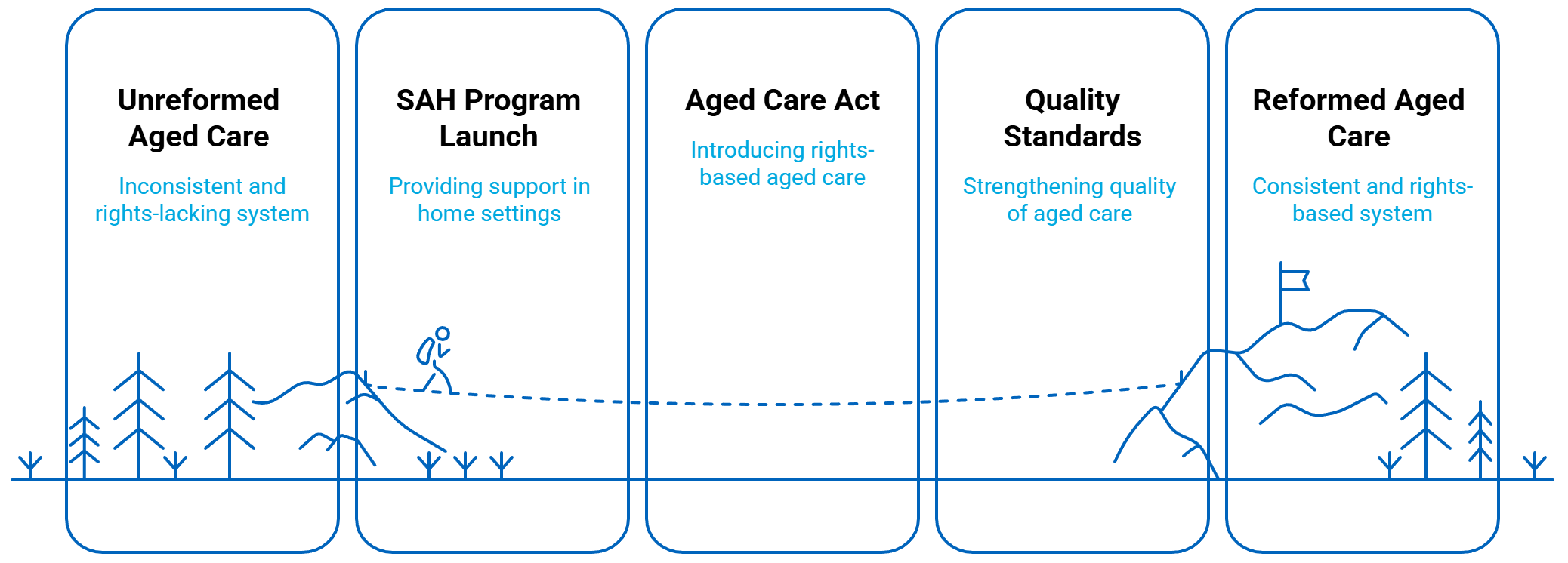
The official commencement of the Support at Home (SAH) Program, alongside the introduction of the new rights-based Aged Care Act and strengthened Quality Standards, marks a pivotal moment in Australian aged care reform.
Driven by the Royal Commission’s recommendations, this shift is essential for delivering person-centred, high-quality care.
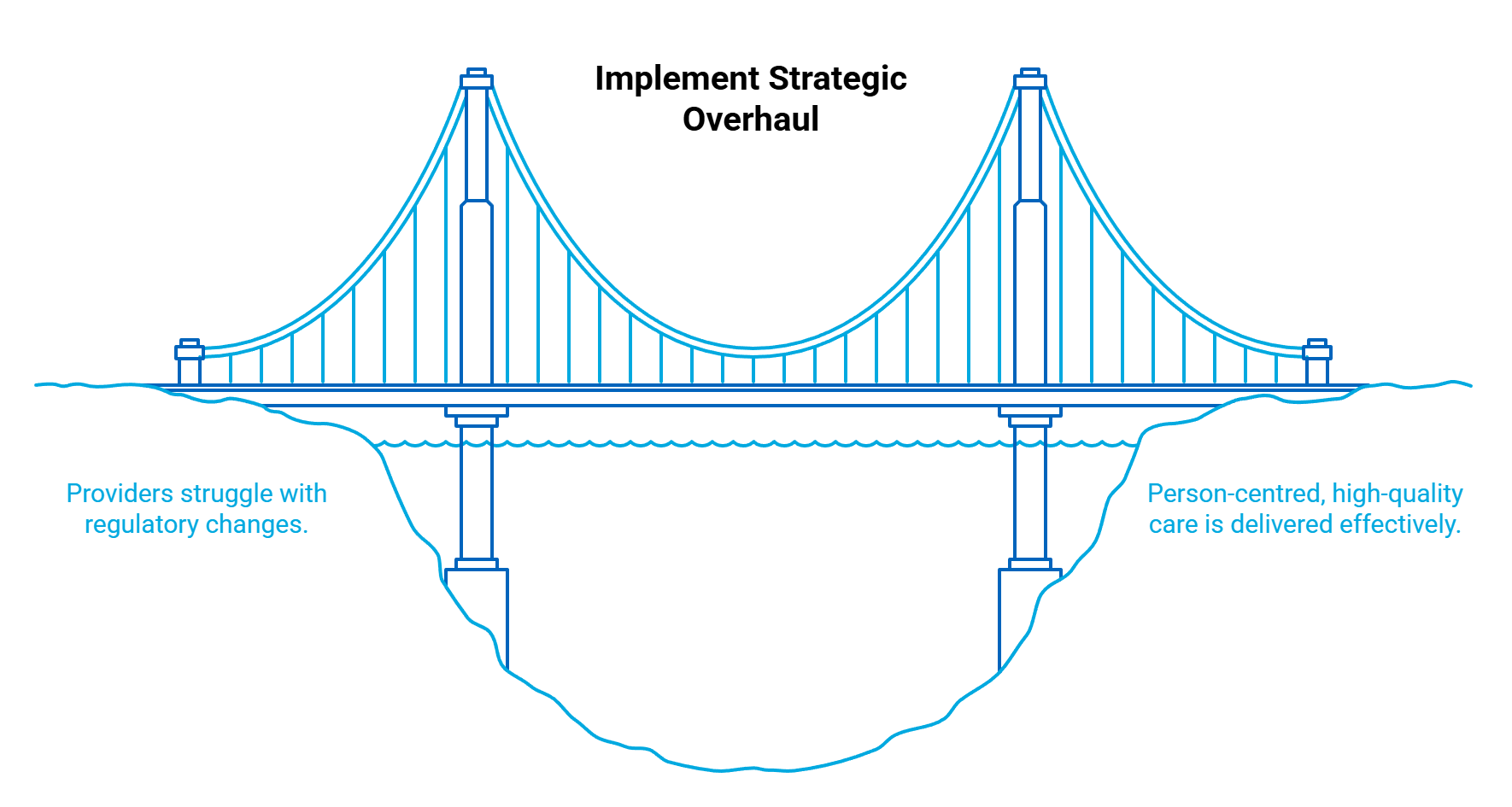
Yet, for registered and associated support providers, the transition is not merely a change in name; it is an immense and costly overhaul, demanding radical adjustments across governance, technology, finance, and culture.
The speed and scale of these necessary changes present distinct, yet interconnected, challenges for all actors in the Support at Home system.
Whilst I won’t attempt to explain every nuance of the transition and challenges in the guide, this article provides an overview of the key challenges for registered and associated Support at Home providers currently.
The Registered Provider’s Compliance and Operational Everest
For registered Support at Home providers, the transition represents nothing short of an institutional rebuild. The scale of the compliance lift alone is staggering, demanding resources that have stressed organisations of all sizes.
The primary challenges include:
- Regulatory Overhaul: Providers must navigate an entirely new Aged Care Act and a set of significantly strengthened Aged Care Quality Standards. This requires deep legal interpretation and integration into daily practice.
- Workforce Education: Ensuring all personnel, from governing persons to front-line workers, including contractors and volunteers, fully understand their new responsibilities and obligations under the Act and Standards is a massive, ongoing training exercise.
- Demonstrating Future Compliance: Achieving readiness for future audits requires a complete realignment of policies, procedures, and shared documentation to demonstrably align with the new regulatory framework.
- Technology Transformation: Standing up and transitioning the necessary software stack is a significant capital undertaking. This technology must be suitable for the Support at Home program, particularly concerning care management, real-time budget management of care plans, and detailed record-keeping.
- New Claiming Practices: Integration with online claiming is required to support efficient claiming practices, which are drastically different from the legacy Home Care Package (HCP) model.
- Brokerage Agreement Restructuring: Registered providers rely heavily on associated providers, necessitating the drafting of new brokerage agreements that clearly articulate compliance obligations and responsibilities under the Act and Standards.
- Pricing Sustainability: Establishing unit pricing and overall fee structures that are appropriate and sustainable for both the registered provider (who will charge their management layer) and the associated provider is a tightrope walk under competitive pressure.
- Change Management and Participant Support: Training all internal staff through this significant change management, supporting existing participants and their families to understand the new model, and managing the signing of new service agreements, including understanding participant contributions, are complex, participant-facing duties.
- Managing Divergent Participant Cohorts: Providers must simultaneously manage grandfathered, transitioning, and new participants, each potentially operating under different rules or funding mechanisms for a transitional period.
The Associated Provider’s Crucible of Cost and Compliance
The complexity for associated providers, those delivering direct services on behalf of a registered provider, varies heavily based on size.
For large associated providers, high compliance requests (provision of clinical notes, auditing, and team member compliance documents) are standard. Furthermore, larger providers have scaled to have the required quality management systems and software to make managing these compliance requirements sustainable.
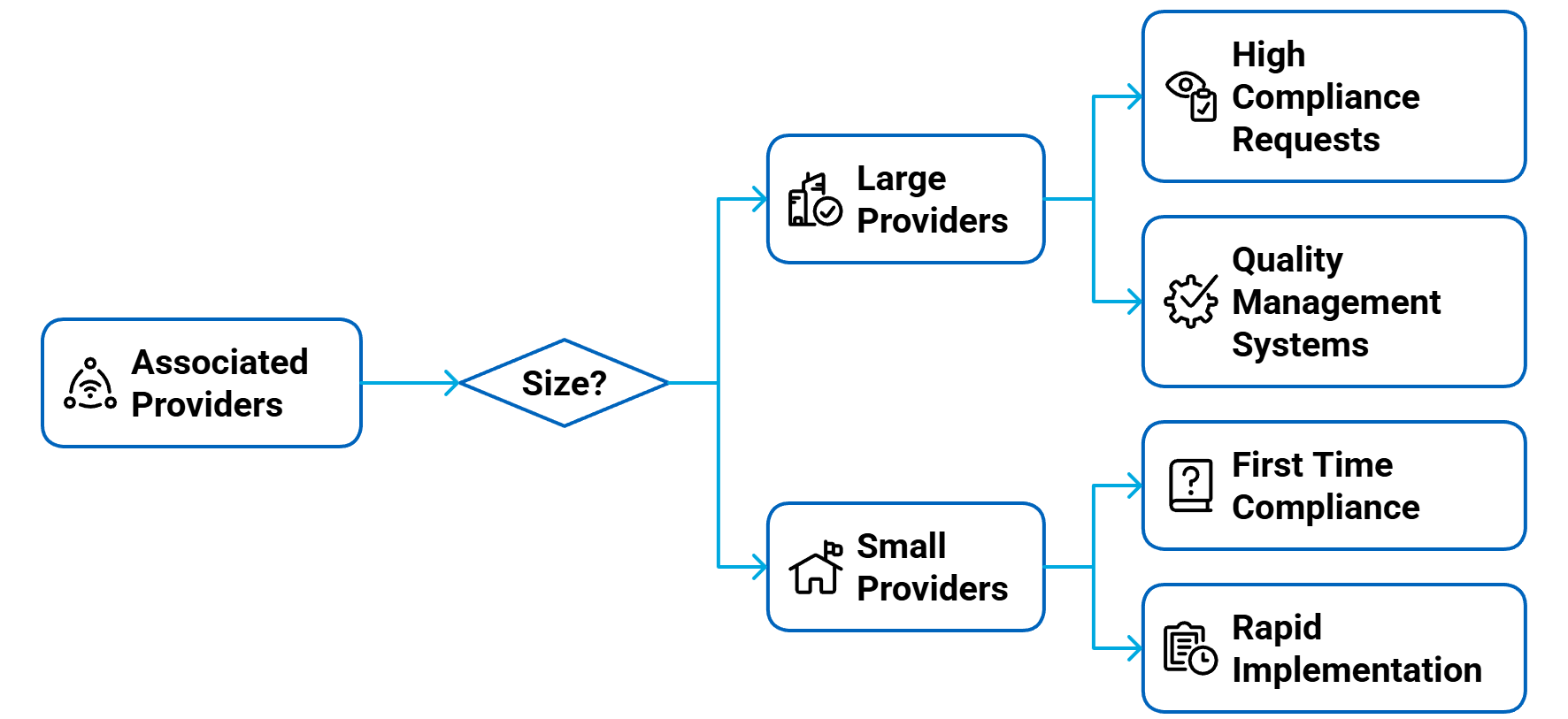
However, for smaller associated providers, this is often the first time they have been subject to such high compliance demands. The speed at which they must absorb and implement this regulatory knowledge is significant.
Associated providers are also grappling with major commercial and administrative shifts:
- Financial Alignment: They must understand how to apply new service codes within their internal software, realign their cost structures, and navigate the government’s pricing guidance and unit prices. The challenge is ensuring their fee structure is sustainable while also aligning with the Support at Home framework and remaining acceptable to registered providers.
- Competitive Pressure: Under Support at Home, registered providers charge their own management fees on top of associated provider fees. This puts intense competitive pressure on associated providers to maintain appropriate, transparent, and lean fee structures.
- Navigating Fragmentation: Associated providers working with multiple registered providers face the administrative challenge of navigating differing interpretations of the Support at Home manual, rules, and compliance requirements from each registered partner. This results in managing multiple service agreements and potentially divergent pricing schedules, creating complexity and inefficiency.
The Inevitable: Expecting Further Change
While the Support at Home program is now officially in effect, history, with the NDIS being a key example, shows that the start of a funding program does not mean the end of change.
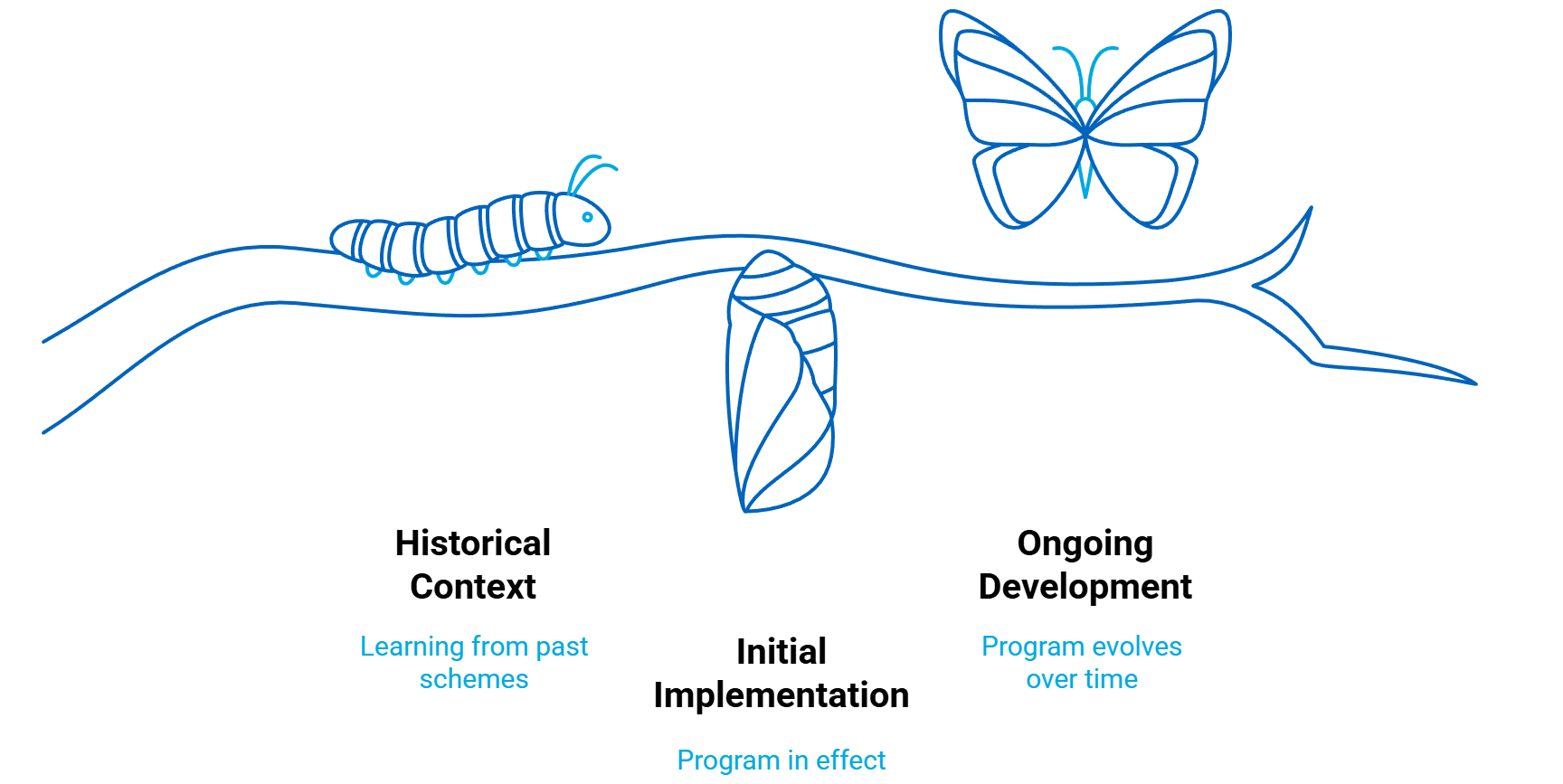
The sector can and should continue to expect significant advocacy and legislative evolution.
The current landscape is marked by two recent Senate inquiries underway, specifically focusing on the transition of the Commonwealth Home Support Program (CHSP) and the critical issue of participant contributions and pricing impacts under the Support at Home program.
With pricing caps expected 1 July 2026, the CHSP due to transition into Support at Home (no earlier than July 2027) and the future program design anticipating a multi-provider model, both registered and associated providers must adopt an expectation of further, constant change across the aged care reform landscape in the short to medium term.
Adaptability is no longer a strategic advantage; it is a prerequisite for survival.


 February 15, 2026
February 15, 2026

